Light therapy, a painless, noninvasive treatment, could significantly lower your risk of vision loss from dry age-related macular degeneration (AMD), according to a study presented at AAO 2024, the annual meeting of the American Academy of Ophthalmology (AAO).1
Researchers revealed that photobiomodulation therapy, a type of light therapy, not only slows the progression of dry AMD but also improves visual acuity in patients. According to lead study author Dr. David S. Boyer, this therapy marks the first effective noninvasive treatment for dry AMD, offering hope to millions who have long struggled with limited options.2
Over two years, patients receiving this light therapy showed remarkable improvements: 53% gained more than five letters in visual acuity, and there was a 73% reduction in new geographic atrophy cases — signifying a significant decrease in the development of advanced damage to the retina — compared to those who didn’t receive the treatment.3 This therapy could soon become a standard, accessible option for preserving your vision without the need for injections or medications.
Understanding Macular Degeneration
AMD is a leading cause of vision loss, particularly affecting individuals over 50. The macula, a small part of your retina, is responsible for sharp, central vision — the clarity you need for reading, driving and recognizing faces. AMD exists in two primary forms: wet and dry.
Wet AMD is characterized by the growth of abnormal blood vessels beneath your retina, which leak fluid and cause rapid vision loss. This form is often managed with anti-vascular endothelial growth factor (anti-VEGF) medications.
In contrast, dry AMD progresses more slowly and involves the thinning and deterioration of your macula without the abnormal blood vessel growth seen in the wet form. Until now, treatment options for dry AMD have been limited to dietary supplements rich in antioxidants and lifestyle changes aimed at slowing the disease’s progression.
The Most Important Way to Prevent AMD
An ounce of prevention is worth a pound of cure, so before I go into the details of light therapy, I want to share the No. 1 way to prevent AMD — a disease process rooted in mitochondrial dysfunction and insulin resistance, triggered by the long-term consumption of seed oils rich in linoleic acid (LA).
Your eyes are highly susceptible to damage caused by polyunsaturated fats (PUFAs) such as LA.4 PUFAs are prone to oxidation, which means the fat breaks down into harmful metabolites, including oxidized LA metabolites (OXLAMs). These go on to cause mitochondrial dysfunction, which is a hallmark of most chronic disease.
Seed oils, including soybean, cottonseed, sunflower, rapeseed (canola), corn and safflower, are present in almost every processed food, including those from restaurants. To avoid it, you’ll need to eliminate most processed foods from your diet. Additionally, LA is hidden in seemingly “healthy” choices like chicken, pork and even olive oil, which is often blended with cheaper seed oils.
To protect your vision and overall health, it’s wise to keep your LA intake below 5 grams per day from all sources. If you can get it below 2 grams, that’s even better. To help you track your LA intake, make it a habit to enter all your foods into a nutrition tracker. That way, you can tally how much LA you’re consuming daily and adjust your meals accordingly.
The Promise of Photobiomodulation Therapy for AMD
Photobiomodulation (PBM) therapy uses specific wavelengths of light to enhance the function of cells in the retinal pigment epithelium (RPE), the layer of cells at the back of your eye that’s necessary for maintaining retinal health.
By improving cellular function, photobiomodulation keeps these cells healthy longer, slowing or even reversing the degenerative processes that lead to vision loss. Unlike conventional treatments, this therapy doesn’t require the discomfort and risks associated with injections or medications.
A study published in the journal Retina also revealed promising results of photobiomodulation therapy for dry AMD.5 This randomized, controlled trial enrolled 100 subjects across 10 U.S. centers. Participants were aged 50 and older, diagnosed with intermediate dry AMD and exhibited best-corrected visual acuity (BCVA) scores between 50 and 75 letters, corresponding to a Snellen equivalent of 20/32 (slightly below normal) to 20/100 (moderately impaired).
Participants were randomly assigned in a 2:1 ratio to receive either the multiwavelength PBM treatment or a placebo treatment. The PBM regimen involved nine treatment sessions over three to five weeks, repeated every four months for a total of six series over 24 months. The placebo treatment mimicked the PBM procedure but with significantly reduced light intensity.
Patients receiving PBM therapy experienced significant improvements. At the 13-month mark, those who received PBM experienced an average increase of 5.4 letters in BCVA, compared to a three-letter gain in the placebo group. This difference is statistically significant and clinically meaningful, especially considering the progressive nature of dry AMD.
Moreover, 55% of the PBM-treated eyes achieved a gain of five or more letters, and 26.4% saw an improvement of 10 or more letters. In contrast, only 40.8% and 15.1% of the placebo-treated eyes achieved these milestones, respectively.6
Stabilizing or even improving vision in early to intermediate stages of dry AMD significantly impacts daily activities and overall quality of life. Additionally, the PBM group showed fewer instances of visual decline, with fewer eyes losing five or more letters compared to the placebo group. These results underscore PBM’s ability to halt and even reverse some of the vision loss associated with dry AMD.
Safety and High Compliance Rates: A Promising Profile
The Retina study provided reassuring data regarding the safety profile of photobiomodulation. Throughout the 13-month period, only 22.3% of treated eyes experienced at least one ocular-specific adverse event, with the majority being mild to moderate in intensity.7 Importantly, no adverse event was reported by more than 5% of participants, and none led to discontinuation of the study.
Compliance rates were impressively high, with 88.2% of PBM-treated eyes fully adhering to the treatment protocol compared to 74.5% in the placebo group. This high level of compliance is indicative of the therapy’s tolerability and the minimal burden it places on patients, with each treatment session lasting less than five minutes per eye.
The favorable safety and compliance data suggest that PBM therapy is well-accepted by patients, making it a viable long-term option. The absence of significant phototoxicity or other severe side effects also positions PBM as a safe alternative to more invasive treatments currently available for AMD.
More Evidence Light Therapy Benefits Dry AMD
A separate study published in Ophthalmology and Therapy also provides compelling evidence on the safety and efficacy of photobiomodulation for treating dry age-related macular degeneration (dAMD).8 This randomized, controlled, double-blind trial involved 76 patients over the age of 50 with dAMD.
Participants were assigned to receive either the PBM treatment or a placebo procedure. The treatment regimen included two cycles of sessions spread over several weeks. At the four-month mark, patients treated with PBM showed a significant improvement in best-corrected visual acuity, with 20.3% achieving a gain of five or more letters compared to 8.9% in the placebo group.
Additionally, there was a notable reduction in drusen volume among the PBM-treated eyes, suggesting that PBM may help slow the accumulation of harmful deposits beneath the retina.
Drusen, yellow deposits under the retina, are a hallmark of AMD and contribute to disease progression. By reducing drusen volume, PBM therapy may help slow the advancement of AMD, delaying the onset of more severe stages like geographic atrophy (GA) or neovascular AMD (nAMD).
Importantly, the study reported minimal adverse events, with only mild ocular discomfort experienced by a fifth of the treated patients. The most common adverse events included mild symptoms like dryness and warmth at the application site, which were easily managed and did not lead to any discontinuations.
Exploring the Biochemical Foundations of Light Therapy
PBM therapy utilizes specific wavelengths of red to near-infrared light (600 to 1,100 nanometers) to target the mitochondria within your retinal cells.9 Mitochondria are the powerhouses of your cells, responsible for producing adenosine triphosphate (ATP), the primary energy source that fuels cellular functions.
When PBM light penetrates your retinal tissue, it’s absorbed by cytochrome c oxidase (CCO), an enzyme in the mitochondrial electron transport chain. This absorption enhances mitochondrial activity, leading to increased ATP production, which in turn boosts cellular metabolism and promotes the repair and regeneration of retinal cells.
Moreover, PBM therapy helps reduce oxidative stress by decreasing the levels of reactive oxygen species (ROS) and mitigating inflammation within the retinal environment.10 The benefits of light therapy also extend to other macular diseases, offering hope for broader vision preservation. One such condition is diabetic macular edema (DME), a complication of diabetes that causes swelling in the macula due to leaking blood vessels.11
Preliminary studies have explored PBM’s effectiveness in reducing retinal thickness and edema in DME patients. Additionally, PBM therapy is being investigated for pachychoroid disorders, a group of diseases characterized by an abnormal thickening of the choroid layer in the eye. Early studies suggest PBM could help reduce inflammation and enhance mitochondrial function in these conditions.12
Photobiomodulation, particularly low-level red-light therapy (LLRL), is also beneficial for myopia, commonly known as nearsightedness.13 A meta-analysis, published in Clinics and involving 685 patients with a mean age of 9.7 years, found that LLRL therapy was associated with better outcomes in two key measures of myopia progression: spherical equivalent refraction (SER) and axial length (AL) change.14
A comprehensive review of multiple studies also found that red light therapy, using wavelengths between 635 to 650 nm, effectively reduces axial elongation of the eye and slows the increase in myopic spherical equivalent refraction, suggesting the nearsightedness is progressing more slowly.15 What’s more, these benefits were observed in treatments ranging from just four weeks up to 24 months.
The Role of the Optical Window in Light Therapy
Understanding the concept of the optical window is fundamental to harnessing the full benefits of photobiomodulation therapy. The sun emits a broad spectrum of light, with over half (53%) falling within the red, near-infrared, mid-infrared and far-infrared wavelengths. These wavelengths are categorized into three main groups:
1. Ultraviolet (UVA, UVB, UVC) — Comprising 7% of the solar spectrum, these wavelengths are responsible for skin tanning.
2. Visible light — Spanning from violet to red (400 to 700 nanometers), visible light accounts for 39% of the spectrum and is essential for vision.
3. Infrared light — Making up the largest portion at 54%, infrared light ranges from 700 to 10,000 nanometers and is invisible to the naked eye.
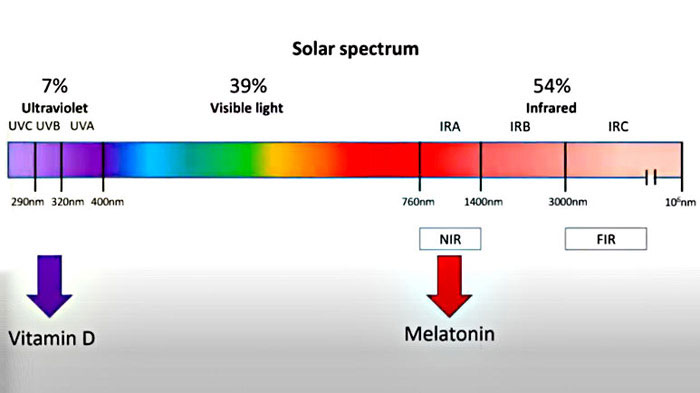
The optical window, specifically between 600 to 1,100 nanometers, is where PBM therapy operates most effectively. This range, particularly around 800 to 810 nanometers, allows light to penetrate deeply into tissues without being significantly absorbed by hemoglobin, melanin or water.
Below 600 nanometers, light penetration is limited as it is readily absorbed by these pigments, reducing its therapeutic reach. By focusing on the optimal optical window, PBM therapy delivers targeted energy to your retinal cells, enhancing cellular function and promoting eye health without unnecessary absorption or scattering.
The Multifaceted Benefits of Near-Infrared Light
Near-infrared (NIR) light plays a pivotal role in the effectiveness of PBM therapy, offering several biochemical advantages that support retinal health. One of the primary benefits of NIR exposure is the significant increase in ATP production within your mitochondria. Enhanced ATP levels boost cellular metabolism, assisting in the repair and regeneration of retinal cells affected by dry age-related macular degeneration.
Additionally, NIR light stimulates the production of melatonin within your mitochondria. While 5% of melatonin is produced by your pineal gland, 95% is generated in your mitochondria and acts as a powerful antioxidant. This melatonin effectively reduces oxidative stress by neutralizing free radicals directly within your mitochondria, protecting them from damage and ensuring their optimal performance.
Furthermore, melatonin helps increase glutathione levels, a vital detoxification agent that eliminates toxins and reduces inflammation.
It also promotes the release of nitric oxide (NO), enhancing blood circulation and vasodilation. These combined effects make near-infrared light a cornerstone of PBM therapy, offering comprehensive support for maintaining and improving retinal health.
Tailoring Your PBM Therapy: Optimal Dosing Strategies
Achieving the best results with photobiomodulation therapy hinges on delivering the right dose of red and near-infrared light. The concept of dosing in PBM is akin to finding the “Goldilocks” zone — not too little to be ineffective, and not too much to cause inhibition. Scientific studies typically utilize doses ranging from 5 to 50 joules per session, where a joule measures the energy delivered in watts per second.
For general health benefits, a balanced approach is recommended. Aim for approximately 25 joules per session, which can be administered using a large PBM panel. This equates to about 10 minutes of exposure to the front of your body and another 10 minutes to the back, totaling 20 minutes per session. This dosage ensures sufficient energy penetration to stimulate cellular processes without overwhelming the tissues.
While natural sunlight provides some near-infrared exposure, many individuals do not spend enough time outdoors to reap these benefits consistently. PBM devices offer a more targeted and controlled way to deliver the necessary wavelengths for optimal health outcomes. For best results, consult with a health care provider experienced in PBM therapy to determine the most appropriate dosing regimen tailored to your unique needs and health goals.
Selecting the Right PBM Device for Maximum Benefits
Choosing the appropriate photobiomodulation device is essential to maximize the therapy’s effectiveness for your specific health needs. PBM devices vary primarily in the wavelengths they emit and their penetration depth. Red light is excellent for treating superficial skin conditions but doesn’t penetrate deeply into tissues.
On the other hand, near-infrared light penetrates much deeper, making it ideal for targeting muscle tissues, enhancing cognitive functions and supporting retinal health in conditions like dry age-related macular degeneration.
For comprehensive benefits, a mixed PBM device that emits both red and near-infrared light offers the best of both worlds. Such devices allow you to address both surface-level and deeper tissue issues simultaneously. However, achieving these combined benefits requires spending about 50% more time using the device compared to using a device that emits only near-infrared light.
When selecting a PBM device, consider factors such as the specific health condition you wish to treat, the required penetration depth and the convenience of incorporating the therapy into your daily routine. Devices with adjustable settings that allow you to customize wavelengths and dosages provide greater flexibility and efficacy.
Additionally, ensure that the device you choose is clinically validated and comes from a reputable manufacturer to guarantee safety and reliability. While avoiding seed oils to protect your vision and prevent AMD is highly recommended, the advancements in light therapy symbolize a significant leap forward in combating vision loss, offering renewed hope and tangible benefits for those affected by dry macular degeneration and other eye conditions.
Test Your Knowledge with Today’s Quiz!
Take today’s quiz to see how much you’ve learned from yesterday’s Mercola.com article.
What dietary change is linked to the decline in metabolic rates in the U.S.?
Source:
articles.mercola.com
Source link

